Early-stage oral tongue squamous cell carcinoma (OTSCC) comprises 25‒40% of oral cancer, and has relatively poorer survival outcomes compared with tumors at other sites. National Comprehensive Cancer Network (NCCN) of the United States and European Head and Neck Society recommend radical surgery as the standard treatment modality for OTSCC, while postoperative radiotherapy (PORT) is not often considered for early-stage OTSCC patients without risk factors, due to the lack of robust evidence.
However, Chair of SAHZU Radiation Oncology Prof. WEI Qichun and his team, for the first time, revealed the critical role of PORT in early-stage OTSCC. Their article titled “Impact of Postoperative Radiotherapy on the Prognosis of Early-Stage (pT1-2N0M0) Oral Tongue Squamous Cell Carcinoma was published” in Journal of Clinical Oncology on April 1.
In their clinical practice, Prof. WEI and his team noticed that these early-stage OTSCC patients easily suffered recurrences after standard treatment. According to statistics, the 5-year recurrence rate of early-stage OTSCC was as high as 21.6%, which seriously affected the survival prognosis of these patients. It suggests that the current treatment modality recommended by the guidelines should be improved.
In their work, the research team conducted a study with world’s largest cohort (528 cases) of early-stage (pT1‒2N0M0) OTSCC. Among these patients, 383 (72.5%) underwent surgery alone, while 145 (27.5%) underwent surgery + PORT. The results demonstrated that PORT was associated with improved survival outcomes on multivariate analyses. On the contrary, moderate-poor differentiation, perineural infiltration (PNI), lymphovascular invasion (LVI), and increasing depth of invasion (DOI) were associated with poorer survival outcomes.
Further subgroup analyses were performed. Researchers found that moderately-poorly differentiated patients had improved overall survival (OS) by 28% and disease-free survival (DFS) by 38% after PORT. Patients with PNI and/or LVI had improved overall survival by 23% and disease-free survival by 29% after PORT. After excluding those with PNI and/or LVI among moderately-poorly differentiated patients, the benefit of PORT was still significant: OS, 97% vs. 82%, P = .040; DFS, 87% vs. 64%, P = .012. In subgroups with DOI > 5 mm, PORT also contributed to improved DFS (80% vs. 64%, P = .006).
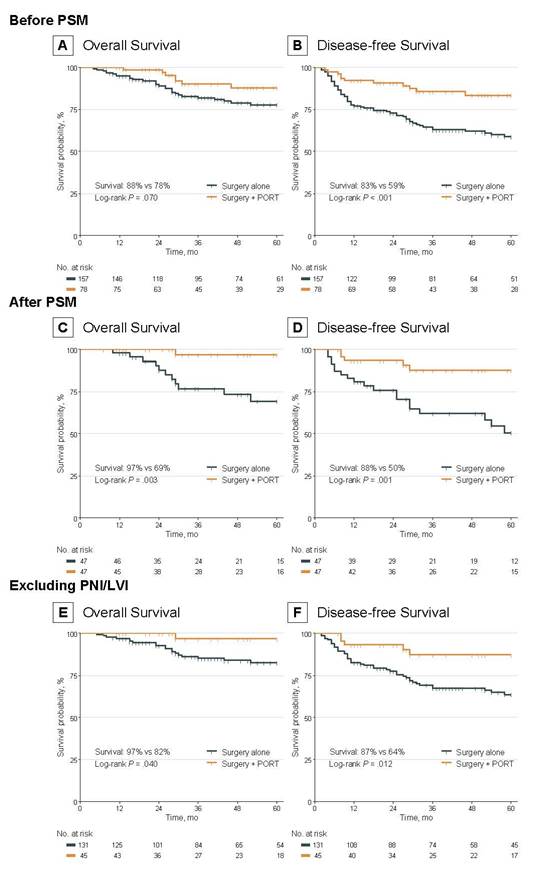
This study sheds, for the first time, that patients with moderately-poorly differentiated early-stage (pT1‒2N0M0) OTSCC benefit from PORT. Also, it provides robust evidence that patients with PNI and/or LVI who undergo PORT have improved survival. And PORT offers DFS benefit among patients with DOI > 5 mm.
These findings, derived from a large sample size, suggest a reconsideration of the current guidelines regarding the application of PORT in patients with early-stage (pT1‒2N0M0) OTSCC.
Source: The Second Affiliated Hospital, Zhejiang University School of Medicine